Translate this page into:
Ruminations, cognitive inflexibility, and their relationship with suicidal ideation in depressive disorders: A neuropsychological approach

*Corresponding author: Dr. Shreekantiah Umesh, Associate Professor of Psychiatry, Central Institute of Psychiatry, Kanke, Ranchi -834006, Jharkhand, India. umesh.yes@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Navya KP, Bose S, Das B, Umesh S. Ruminations, cognitive inflexibility, and their relationship with suicidal ideation in depressive disorders: A neuropsychological approach. Arch Biol Psychiatry 2023;1:19-24.
Abstract
Objectives:
Depression is theorized to result from “cognitive constriction” and problem-solving deficits, making an individual vulnerable to suicidal thoughts and acts. The present study explored the relationships between metacognitive beliefs, ruminations, and executive functions in patients with depression with suicidal ideation and without suicidal ideation.
Material and Methods:
Fifty patients of clinical depression (n = 25 depression with suicidal ideation, n = 25 depression without suicidal ideation) were recruited using purposive sampling. All participants completed the sociodemographic data sheet, Modified Scale for Suicidal Ideation, Metacognition Questionnaire 30, Ruminative Response Scale, Cognitive Flexibility Scale and Hamilton Rating Scale for Depression, and executive functions tests such as Wisconsin Card Sorting Test and Eriksen Flanker Test.
Results:
Metacognition and rumination responses were significantly higher in patients with depression with suicidal ideation than in patients without suicidal ideation. In addition, cognitive flexibility is higher in patients with depression without suicidal ideation, and executive deficits were higher in depression with suicidal ideation than without suicidal ideation.
Conclusion:
The findings support the role of metacognitive beliefs, ruminations, and executive deficits in maintaining suicidal ideations in depression.
Keywords
Depression
Suicidal ideation
Neuropsychological variables
Cognitive flexibility
INTRODUCTION
Major depressive disorder is a mental disorder characterized by low mood, decreased energy, and loss of interest or pleasure in normally enjoyable activities. This disorder affects an estimated 264 million people and is currently the leading cause of disability.[1] According to the National Mental Health Survey conducted in India, one in every 20 people aged 18 and up suffers from clinical depression, 51% have some level of suicidality, and 3% have attempted suicide in the previous month.[2] Suicidal behavior is frequently the result of a person’s perception of an overwhelming situation. It can happen due to a variety of risk factors such as psychological trauma, unemployment, financial crisis, guilt feelings, substance abuse, personality psychopathology, and so on. Ruminative thinking, hopelessness, poor problem-solving, metacognition, and cognitive inflexibility have all been identified as risk factors for suicidal ideation and attempts in young adults.[3] Cognitive inflexibility is defined as the inability to change decisions in response to environmental feedback.[4] Depression has been hypothesized being the result of cognitive constriction and problem-solving deficits, which makes a person vulnerable to suicidal ideations. People who are cognitively restrictive, are unable to find effective solutions to stressful situations, which increases the risk of suicidal behavior.[5] Depressive rumination is defined as a response mode, in which individuals focus on distress symptoms and the possible causes and outcomes of such symptoms repeatedly and passively.[6] It is consistently reported in depressive disorders and is correlated with the severity of the illness and is an important predictor of suicidal behavior.[7] Furthermore, rumination has also been studied in relation to cognitive inflexibility. Previously, a study discovered that people with higher trait rumination were more cognitively inflexible and made more perseverative errors on the Wisconsin card sorting test (WCST) than people with low trait rumination.[6] Furthermore, rumination is linked to poor problem-solving, which is thought to be the result of cognitive inflexibility. Ruminations deplete cognitive resources, making it difficult to complete tasks that require adequate attention and executive functions. Ruminators have difficulty suppressing irrelevant memories or inhibiting prepotent responses, according to research. Rumination causes increased interference from automatic tendencies on tasks such as the Stroop and Eriksen Flanker task, and executive overload may result in poorer performance on these tasks.[8]
Wells’ metacognitive theory of emotional disorders includes the cognitive-attentional syndrome (CAS). CAS is a set of psychological processes that include repetitive negative thinking (worry and rumination), threat monitoring, and associated disobliging behavioral and cognitive strategies; it is derived from metacognitive beliefs, which can be positive or negative. While most people have brief periods of negative self-appraisal, the prolonged occurrence of negative emotions and negative self-appraisal in some people is due to CAS activation which may further activate syndromal depression.[9]
There is, however, a need to understand the interactive role of the attentional processes and executive control on cognitive inflexibility and rumination, thereby harboring suicidal thoughts. The primary goal of this study was to better understand the psychological (rumination and cognitive inflexibility) and neuropsychological (selective attention and executive control) correlates of suicidal ideation in unipolar depression patients. We also hypothesized that depressed patients with higher suicidal ideation (DSI) would be more ruminative and cognitively rigid than depressed patients with no suicidal ideation (NSI). Finally, we hypothesized that the DSI group might perform worse on attention and executive functions than the NSI group.
MATERIAL AND METHODS
Participants and procedure
Fifty patients with a diagnosis of depressive disorder as per ICD-10 DCR.[10] Criteria with no comorbid medical/ psychiatric disorders were recruited from the outpatient department of Psychiatry and Psychosocial Unit of Clinical Psychology, Central Institute of Psychiatry, Ranchi, Jharkhand using purposive sampling. Individuals who received or have received electroconvulsive therapy in the past 6 months were excluded from the study. The data collection was started on April 2021 and ended in August 2021. A written informed consent was taken from all the participants who agreed to take part in the study. Patients who had active suicidal ideation (score more than 9 in MSSI) were included in DSI group (n = 25), who does not have active suicidal ideation (score <9 in MSSI) were included in NSI group (n = 25). All the participants age ranged between 18 and 45 years. Each participants were asked to complete the sociodemographic data sheet, MSSI;[11] Hamilton Rating Scale for Depression (HRSD or HAM-D);[12] Ruminative Response Scale (RRS);[13] Cognitive Flexibility Scale (CFS);[14] and executive functions tests such as WCST[15] and Eriksen Flanker Test.[16] The ethical committee of the institute approved the study, and it was conducted in accordance with the Declaration of Helsinki.
Measures
MSSI – The MSSI is an 18-item scale that helps to assess the severity of suicidal ideation over a 48-h period. The scale determines intention, competence to attempt suicide, and amount of talking/writing about death. The suicide item has been found to have good reliability and validity for assessing suicidality.
HAM-D – The HDRS (also known as the HAM-D) is the most widely used clinician-administered depression assessment scale developed by Max Hamilton in 1960. The original version contains 17 items (HDRS-17) pertaining to symptoms of depression experienced over the past week. Results are categorized as mild, moderate, or severe depression.
RRS – The RRS is a 22-item measure of proneness to ruminative thought when feeling sad or low. A total score can be calculated, as well as subscale scores for “brooding” and reflective pondering. Adequate psychometric properties were reported including good internal consistency, moderate test-retest reliability, and evidence for construct validity for the total score and subscale scores.[17]
The CFS is a 12-item self-report scale (6-point Likert scale: 1 = strongly disagree to 6 = strongly agree) that assesses the aspects of cognitive flexibility considered relevant for (1) awareness of options, (2) willingness to be flexible, and (3) self-efficacy in being flexible (Martin and Rubin, 1995). Each item on the questionnaire consists of a statement dealing with beliefs and feelings about behavior. A higher score indicates more cognitive flexibility.
WCST – The WCST was developed by Heaton and colleagues. It is used to measure cognitive functions mainly executive control. The test included two decks of cards with four stimulus cards and 64 reaction cards. There is no time limit and the total number of errors, perseverative errors and non-perseverative errors. The completed categories were used to determine cognitive flexibility.
Eriksen Flanker Task – Flanker card is a set of response inhibition tests. It is used to find the ability to suppress responses in a particular inappropriate context. The target of the test is flanked by non-target stimuli which corresponded either b the same directional response as the target (congruent), to the opposite response (incongruent) or to neither (neutral). In this test, a directional response (left or right) considered a central target stimulus. Incongruent, congruent, neutral stimuli represented by arrows. We used psychology experiment-based language software 2.0 Beta 4 (open source) for this test which was provided on a 15’ laptop screen at a distance of one meter.[18]
Statistical analyses
We used descriptive statistics for analyzing the sociodemographic and clinical characteristics of the samples. We used Q-Q plots to visualize the distribution of the data. Pearson correlation coefficient and multiple linear regression analysis was used to understand the association of various factors to suicidal ideation. Finally, we used the independent sample t-tests for comparison of DSI and NSI groups. We used SPSS 20® for Windows® for the statistical analysis.
RESULTS
[Table 1] shows sociodemographic and clinical characteristics of the samples. The samples were predominantly men (62%), married (62%), and Hindu (86%). Mean age of onset was 28.72 ± 7.34 years, the duration of the current episode was 4.74 ± 2.25 months, and samples were having higher proportion of recurrent depressive disorders as the diagnosis (64%).
| Sociodemographic variables | Mean/SD or n/n% |
|---|---|
| Age (in years) | 32.34±9.12 |
| Gender | |
| Men | 31 (62) |
| Women | 19 (38) |
| Religion | |
| Hindu | 43 (86) |
| Others | 7 (14) |
| Domicile | |
| Urban | 27 (54) |
| Rural | 23 (46) |
| Years of education | 12.80±3.06 |
| Marital status | |
| Married | 31 (62%) |
| Unmarried | 19 (38) |
| Clinical variables | |
| Age of onset of illness (in years) | 28.72±7.34 |
| Recurrent depressive episodes | |
| Present | 32 (64) |
| Absent | 18 (36) |
| Number of past episodes | |
| Single episode | 19 (38) |
| Two episodes | 09 (18) |
| Three episodes | 03 (06) |
| Four or more | 01 (02) |
| Duration of current episode (in months) | 4.74±2.25 months |
| Family history of depressive disorder | |
| Absent | 38 (76) |
| Present | 12 (24) |
Correlations of the study variables are presented in [Table 2]. Suicidal ideation was positively correlated with depression and both brooding and reflective rumination styles as expected. Furthermore, suicidal ideation was positively correlated to rumination (total score) and negatively correlated with cognitive flexibility (total score) [Figure 1]. Among the neuropsychological variables, only category completed on WCST was negatively correlated with suicidal ideation (r = −0.28, P = 0.042). No other neuropsychological variables were significantly correlated with suicidal ideation. Stepwise multiple linear regression analysis was conducted to determine the predictors of suicidal ideation in the sample. In step three of regression equation, suicidal ideation accounted for 62.9% variance. The variables main effects of F (1, 49) = 28.63, P < 0.001***, β = 0.39, t (49) = 3.37, P< 0.002** was found with severity of depression, β = 0.48, t (49) = 4.01, P < 0.001*** for rumination and β =−0.25, t (49) = −2.78, P < 0.008** for incongruent reaction time in Eriksen Flankers task.
| Suicidal ideation | Severity of depression | Rumination | Brooding | Reflection | Cognitive flexibility | |
|---|---|---|---|---|---|---|
| Suicidal ideation | 1 | |||||
| Severity of Depression | 0.71** | 1 | ||||
| Rumination | 0.61** | 0.64** | 1 | |||
| Brooding | 0.57** | 0.55** | 0.58** | 1 | ||
| Reflection | 0.52** | 0.53** | 0.59** | 0.54** | 1 | |
| Cognitive flexibility | −0.29* | −0.27 | −0.37** | −0.24 | −0.24 | 1 |

- The scatterplot illustrates the positive linear relationship of suicidal ideation and negative linear relationship with cognitive flexibility.
Finally, we conducted a subanalysis by comparing the psychological and neuropsychological variables between the two groups (DSI and NSI) based on the MSSI cutoff score = 9. Results of independent sample t-tests show significantly higher rumination (t = 5.75, P < 0.001***) and lower cognitive flexibility (t = −2.56, P = 0.014*) in DSI group as compared to NSI group [Figure 2a]. DSI group had significantly higher rates of perseverative errors as compared to NSI on WCST (t = 5.71, P = 0.008**) and significantly higher errors on identifying both congruent and incongruent trials of EFT (t = 2.30, P = 0.026*) [Figure 2b and c]. Other psychological and neuropsychological variables were non-significant.
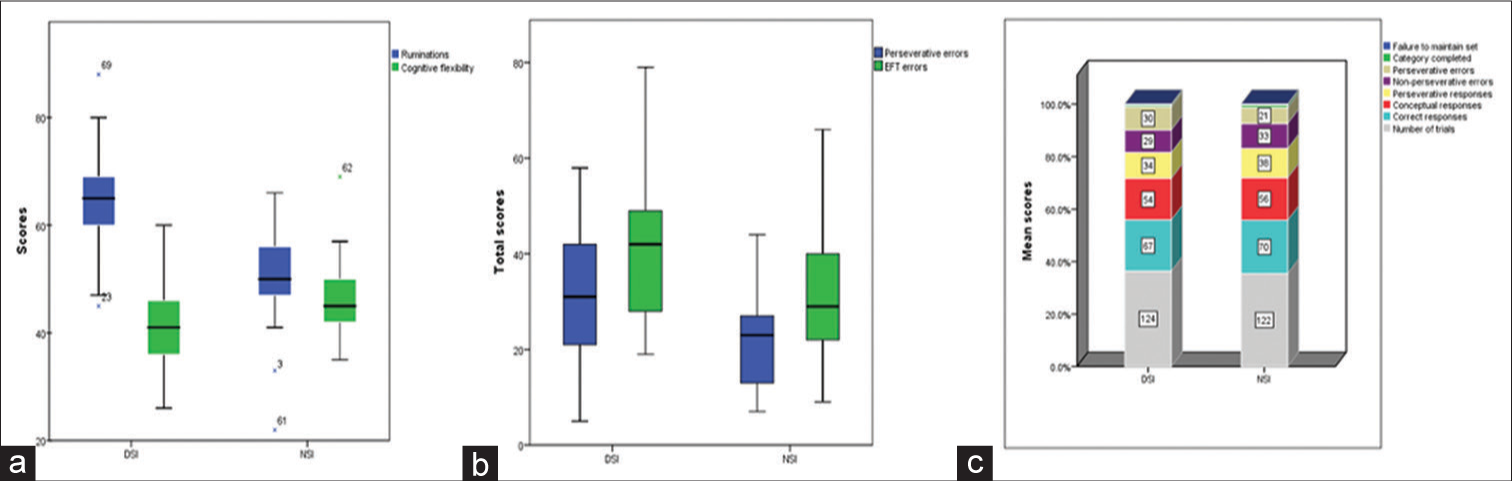
- The boxplots shows that comparison of ruminations and cognitive flexibility (a) and errors on neuropsychological tests (b) between DSI and no suicidal ideation (NSI) group. (c) The clustered bar graph of performance on Wisconsin card sorting test between DSI and NSI group. The mean scores of DSI group were higher on the perseverative and EFT errors as compared to NSI group.
DISCUSSION
The present study aimed to investigate the relationship of suicidal ideation with various psychological and neuropsychological variables in patients with depressive disorders. The study has strengthened the previous research findings which highlighted a linear relationship with ruminations and cognitive flexibility in patients harboring suicidal ideations.[4,7] Using neuropsychological variables of attentional as well as executive control have provided newer findings to the existing literature.[19] The findings show that patients with depression who have suicidal ideation are cognitively less flexible, as evidenced by an inability to change decisions in response to feedback from the environment in lines with the previous literature.[20] The CAS consists of worry, rumination, fixated attention, and unhelpful self-regulatory strategies or coping behaviors and rumination was found to be more for patients of depression with suicidal ideation.[9,21-23] The domains of depression related items and brooding was significantly high in with higher suicidal ideation. These results are consistent with a prior finding that brooding predicted increases in depression.[17] Brooding may be associated with increases in thoughts of suicide because it involves attention to painful symptoms of depression and the negative consequences of depression[24] Moreover, patients of depression without suicidal ideation group took significantly a smaller number of trials to complete WCST categories and they were given a greater number of correct response and conceptual level response than with suicidal ideation group. The preservative errors (number of errors in which a subject continuously responds incorrectly using the same pattern) were higher in the DSI as compared to NSI group. Earlier King et al.[19] found depressed suicide attempters performed worse with age in terms of mental sequencing and flexibility than depressed non-attempters (Trail Making Test, part B, Time and Sequencing). Interestingly, they found no differences between groups on tests of attention/concentration, verbal or figural fluency, or another test of mental flexibility and abstract reasoning. On the contrary, impaired EF and suicidality are associated with difficulties in decision making[25] and impulsivity.[26]
This study also reveals that a significant difference in errors during performance of the Flanker card task in DSI as compared to NSI group. The DSI group performed with a greater number of errors and less reaction time, that is, they quickly responded to the stimulus which amounts to impulsivity being common in those with prominent suicidal ideation.[26] It appears that rumination magnifies depressive symptoms, suicidal ideation, and likelihood of attempts by keeping the negative cognitions associated with depressed mood. On further, activation of such vicious circle may interfere with effective problem solving by encouraging a passive and pessimistic state. Overall, our study finding provides a framework to the role played by rumination and cognitive inflexibility, further by state-dependent neuropsychological deficits may trigger suicidal ideation and may lead to future attempt.
CONCLUSION AND FUTURE DIRECTIONS
The present study concludes that ruminations and cognitive inflexibility are associated with suicidality in patient with depression. Moreover, state-dependent neuropsychological deficits in attentional and executive control may worsen depression which may predict suicidal ideation. Major limitations of this study are the smaller sample size, correlational study design, predominantly male, which may limit the generalizability. Future studies may focus on the longitudinal studies to assess the trait level presence or absence of these psychological and neuropsychological variables which may relate to suicidal ideation or attempt in patients with depressive disorders.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789-858.
- [CrossRef] [PubMed] [Google Scholar]
- A population-based analysis of suicidality and its correlates: Findings from the National Mental Health Survey of India, 2015-16. Lancet Psychiatry. 2020;7:41-51.
- [CrossRef] [PubMed] [Google Scholar]
- Cognitive vulnerability to depression, rumination, hopelessness, and suicidal ideation: Multiple pathways to self-injurious thinking. Suicide Life Threat Behav. 2006;36:443-54.
- [CrossRef] [PubMed] [Google Scholar]
- Difference in cognitive flexibility between passive and active suicidal ideation in patients with depression. Neuropsychiatry. 2018;8:1000446.
- [Google Scholar]
- Cognitive inflexibility as a prospective predictor of suicidal ideation among young adults with a suicide attempt history. Depress Anxiety. 2012;29:180-6.
- [CrossRef] [PubMed] [Google Scholar]
- Cognitive inflexibility among ruminators and nonruminators. Cogn Ther Res. 2000;24:699-711.
- [CrossRef] [Google Scholar]
- Suicide-Specific Rumination Relates to lifetime suicide attempts above and beyond a variety of other suicide risk factors. J Psychiatr Res. 2018;98:78-86.
- [CrossRef] [PubMed] [Google Scholar]
- An attentional scope model of rumination. Psychol Bull. 2013;139:1036-61.
- [CrossRef] [PubMed] [Google Scholar]
- Neural correlates of cognitive-attentional syndrome: An fMRI study on repetitive negative thinking induction and resting state functional connectivity. Front Psychol. 2019;10:648.
- [CrossRef] [PubMed] [Google Scholar]
- The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research In: Diagnostic Criteria for Research. Geneva: World Health Organization; 1993.
- [Google Scholar]
- The modified scale for suicidal ideation: Reliability and validity. J Consult Clin Psychol. 1986;54:724-5.
- [CrossRef] [PubMed] [Google Scholar]
- A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56-62.
- [CrossRef] [PubMed] [Google Scholar]
- A prospective study of depression and posttraumatic stress symptoms after a natural disaster: The 1989 Loma Prieta Earthquake. J Pers Soc Psychol. 1991;61:115-21.
- [CrossRef] [PubMed] [Google Scholar]
- Wisconsin Card Sorting Test (WCST): Manual: Revised and Expanded Florida: Psychological Assessment Resources (PAR); 1993.
- [Google Scholar]
- Effects of noise letters upon the identification of a target letter in a nonsearch task. Percept Psychophys. 1974;16:143-9.
- [CrossRef] [Google Scholar]
- Rumination reconsidered: A psychometric analysis. Cognit Ther Res. 2003;27:247-59.
- [CrossRef] [Google Scholar]
- The psychology experiment building language (PEBL) and PEBL test battery. J Neurosci Methods. 2014;222:250-9.
- [CrossRef] [PubMed] [Google Scholar]
- A neuropsychological comparison of depressed suicide attempters and nonattempters. J Neuropsychiatry Clin Neurosci. 2000;12:64-70.
- [CrossRef] [PubMed] [Google Scholar]
- Considerations for using the Wisconsin Card Sorting Test to assess cognitive flexibility. Behav Res Methods. 2021;53:2083-91.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of dysphoria and rumination on cognitive flexibility and task selection. Acta Psychol (Amst). 2013;142:323-31.
- [CrossRef] [PubMed] [Google Scholar]
- The cognitive attentional syndrome: Examining relations with mood and anxiety symptoms and distinctiveness from psychological inflexibility in a clinical sample. Psychiatry Res. 2013;210:215-9.
- [CrossRef] [PubMed] [Google Scholar]
- Metacognition, rumination and suicidal ideation: An experience sampling test of the self-regulatory executive function model. Psychiatry Res. 2021;303:114083.
- [CrossRef] [PubMed] [Google Scholar]
- Brooding, inattention, and impulsivity as predictors of adolescent suicidal ideation. J Abnorm Child Psychol. 2019;47:333-44.
- [CrossRef] [PubMed] [Google Scholar]
- Impaired decision making in suicide attempters. Am J Psychiatry. 2005;162:304-10.
- [CrossRef] [PubMed] [Google Scholar]
- Current psychiatric morbidity, aggression/impulsivity, and personality dimensions in child and adolescent suicide: A case-control study. J Affect Disord. 2008;105:221-8.
- [CrossRef] [PubMed] [Google Scholar]








